

Scleroderma
Are you suffering from scleroderma?
Scleroderma is a chronic autoimmune disease that affects your skin, connective tissues, muscles, bones, blood vessels, joints, and organs. It occurs when the immune system triggers your body to produce too much collagen. Collagen is a protein that strengthens skin and provides firmness and elasticity. When you have scleroderma, it causes your skin to become thick and hard, and it’s possible for scar tissue to develop in your lungs, kidneys, and other organs.
According to the Scleroderma Foundation, approximately 300,000 people in the United States have scleroderma disease. Scleroderma can affect people of any age, but it’s most common in people between the ages of 25 and 55. It can take time to receive a scleroderma diagnosis, especially since there is not a specific scleroderma test and the symptoms are similar to many other diseases.
REQUEST NOWWhy do people develop scleroderma?
Unfortunately, doctors have not been able to identify any unique scleroderma causes. Research suggests that the immune system causes an inflammatory response in the body that affects the skin, connective tissues, and organs. More research is needed to determine the exact cause and hopefully prevent more cases from occurring.
What are the most common scleroderma symptoms?
Scleroderma symptoms can vary from person to person and are dependent on which areas of the body are affected. For many people, scleroderma causes areas of thickened, hardened skin on the body. Many other symptoms can occur that affect other parts of the body. These include:
- Dry, itchy skin
- Joint pain and stiffness
- Swelling of the hands and feet
- Muscle weakness
- Sores on your fingertips or toes
- Red spots on the skin
- Trouble swallowing
- Chronic cough
- Shortness of breath
- Sensitivity to cold
- Heartburn
- Digestive and gastrointestinal problems
- Unexplained weight loss
Since there is not a specific scleroderma test used to diagnose the condition, your doctor may ask about your medical history, the scleroderma symptoms you’re experiencing, and perform a physical exam to make a diagnosis. Your doctor might also order blood tests, X-rays, lung function tests, or a CAT scan.
Are there different types of scleroderma?
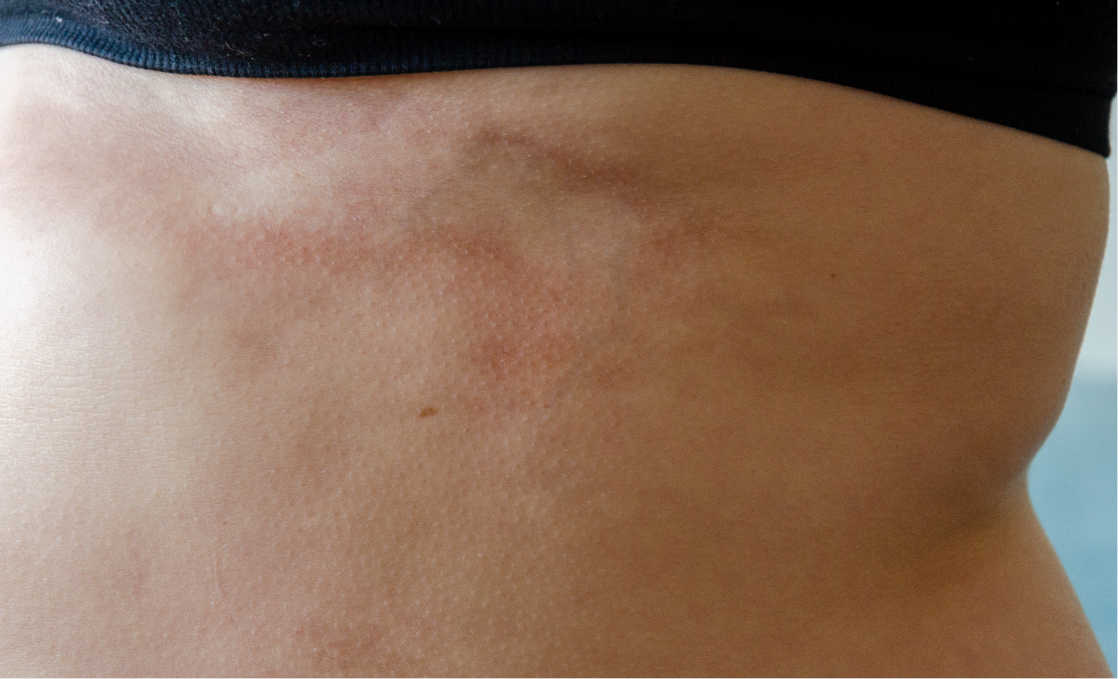
Localized and systemic are the two main types of scleroderma disease. Localized scleroderma is a milder form of the disease. This type usually only affects the skin, but it can spread to your joints, muscles, or bones. There are two types of localized scleroderma – linear or morphea. Linear scleroderma appears as lines or streaks of waxy, hardened skin, typically on the arms, legs, or forehead. If you have morphea scleroderma, you might notice oval-shaped patches of discolored skin.
Systemic scleroderma is more serious, and it can affect the skin, connective tissues, blood vessels, muscles, and organs. This includes the heart, lungs, kidneys, and gastrointestinal tract. Limited and diffuse are the two forms of systemic scleroderma.
Limited scleroderma commonly affects the skin of your feet, hands, and face, and it can also damage your esophagus, intestines, and lungs. It is sometimes called CREST syndrome since it causes these five common symptoms:
- Calcinosis: This occurs when calcium deposits under the skin, causing nodules to develop on your skin or organs.
- Raynaud’s phenomenon: This condition causes a lack of blood flow to specific parts of the body, usually as a response to cold temperatures or stress. It commonly affects the fingers and toes, causing the skin to turn blue, white, or red.
- Esophageal dysfunction: This can cause heartburn or difficulty swallowing.
- Sclerodactyly: If you have sclerodactyly, the skin on your fingers and toes thickens and tightens, causing difficulty with movement.
- Telangiectasia: This causes dilated blood vessels near the surface of your skin, resulting in red spots on your face, fingers, or other areas of the body.

Diffuse scleroderma develops rapidly and causes thickened skin to develop on your arms, legs, hands, feet, and torso. It can also cause significant organ damage, including the lungs, gastrointestinal tract, and kidneys.
What scleroderma treatment options exist for patients?
Although there is not a cure for scleroderma, there are several scleroderma treatment options that can help you control and manage your symptoms. Treatment is based on the symptoms you are experiencing and which tissues or organs are affected.
Topical treatments can be helpful in managing the skin problems that occur with localized scleroderma. Moisturizers can treat and improve hardened skin and can also reduce dryness and itchiness. Applying corticosteroid creams or taking a steroid medication can reduce swelling and inflammation, loosen stiff skin, and slow the progression of further skin changes. To promote the healing of sores on your fingers or toes, your dermatologist may prescribe nitrates to improve blood flow.
Nonsteroidal anti-inflammatory drugs (NSAIDs), such as aspirin or ibuprofen, can help you manage joint pain. To treat Raynaud’s phenomenon, calcium channel blockers or vasodilators can help relax and open the blood vessels. It is also important to ensure that your body is warm, especially your fingers and toes.
Scleroderma treatment also includes physical therapy and regular exercise, which can improve circulation, muscle strength, and help keep your joints flexible. Over-the-counter and prescribed medication can help control heartburn and other digestive problems.
If you are suffering from Scleroderma, get in touch with one of our experienced dermatologists to get started on an effective treatment plan. We are here to help you minimize discomfort and protect your body from further damage. Call our office today to schedule an appointment.
Interested in Scleroderma? Request a consultation with a skin specialist today.
*Treatment options may vary at each location.Please confirm your desired treatment is offered at your preferred location when scheduling. *Age Restriction.
For patients scheduling who are under 18 years of age (19 in Alabama and Nebraska) please make sure you have permission from your parent or legal guardian to schedule this appointment. Your parent or legal guardian must accompany you on your initial visit and on certain subsequent visits to provide appropriate informed consent.